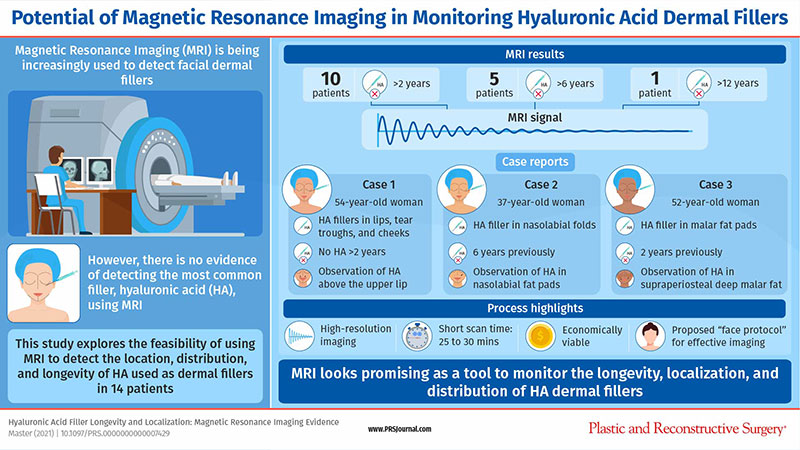
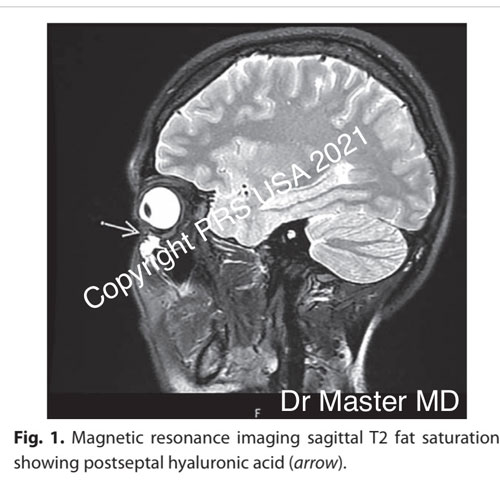
A novel image-guided treatment of postseptal intraorbital complications of dermal filler injection may help to avoid oculoplastic surgery. This article describes three patients who had postseptal hyaluronic acid confirmed by magnetic resonance imaging. All three patients underwent hyaluronidase treatment using a “magnetic resonance imaging road map” and ultrasound-guided dissolution.
This article demonstrates a novel approach using magnetic resonance imaging to identify and treat inadvertent postseptal complications of hyaluronic acid tear trough treatment in three patients. A 25-gauge needle was inserted in the postseptal component under ultrasound guidance with 80 to 100 units of hyaluronidase (Hylase; Sanofi, Paris, France).
The intralesional ultrasound-guided injection of 80 to 100 IU of hyaluronidase (ultrasound-guided injection) was performed with an ultrasound scanner (Precision Pure; Toshiba, Minato-ku, Tokyo, Japan) and an 18-Mhz, high-frequency probe. All magnetic resonance imaging scans and ultrasound-guided procedures were interpreted and performed by one dual-trained aesthetic physician and radiologist with more than 16 years of specialist experience.
In case 1, a 30-year-old woman had tear trough treatment with 0.25 ml/side of Restylane Volyme (Galderma, Switzerland) hyaluronic acid (technique unknown). Two months later, an additional 0.25 ml of Restylane Volyme was blended on each side (technique unknown). The right tear trough had a poor outcome, with lumpiness and significant malar edema directly after the procedure. Numerous hyaluronidase injections were performed, with up to 1500 IU of hyaluronidase per session in the right tear trough area clinically over a 12-month period, with no clinical resolution. Magnetic resonance imaging was performed, showing postseptal hyaluronic acid (Fig. 1). Ultrasound-guided injection of hyaluronidase was performed. Repeated magnetic resonance imaging demonstrated almost complete dissolution of the postseptal hyaluronic acid (Fig. 2). This patient then underwent surgery, as the medial sub–orbicularis oculi fat approaching the inner canthus was resistant to hyaluronidase treatment.